Straight Talk from ex-CDC for the Long Slog Ahead
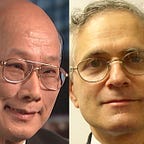
By Bruce G. Weniger, MD, MPH and Chin-Yih Ou, PhD, medical epidemiologist and research-laboratory specialist, respectively; both retired from CDC (link for free, direct, future access to this essay and the final update of its graphs) (link to Rachel Maddow Show interview about this essay) _ _ _ _ _ _ _ [The authors have ceased updating the two figures and the Analyzed Data Table upon the final interval 2022–12–30 to 2023–01–01.] _ _ _ _ _ _ _ [CLICK FIGURES FOR INCREASED SIZE AND LEGIBILITY.]
SINCE its wartime creation in the 1940s to study and control malaria in the South, the agency now known as the Centers for Disease Control and Prevention has been at the global forefront in responding to innumerable threats to public health. But that role for the COVID-19 coronavirus pandemic ended once CDC’s accomplished epidemiologist, Dr. Nancy Messonnier, recounted in a press briefing on February 25th a breakfast discussion presciently warning her children of the pandemic’s “significant disruption of our lives”.
The last COVID-19 press briefing by her or by any other career CDC scientist was on March 9, denying a worried public straight talk from what has been the world’s premier public-health agency. Pandemic messaging and guidance now pass through the political filters of the White House, where reporters’ questions are interrupted mid-stream, political appointees answer with obligate flattery on how well the response is being led, and Q&As with scientists Drs. Anthony Fauci and Deborah Birx are aborted when the politicians abruptly leave the room.
As retirees from an agency whose mission we are proud to have served, we offer some insider views as context for the current crisis, as well as technical insights, suggestions, and questions that former colleagues are now unable to address publicly. First, a little history.
Budget Wars and Ideology
In an alcove of the CDC museum here in Atlanta are posters about the major epidemics investigated by graduates of the Epidemic Intelligence Service — the disease detectives chronicled so well by Berton Roueché. An exception is the 1980–82 cohort’s “Budget Wars”, a takeoff on the sci-fi franchise of that era. The poster annotation and its skit tragicomically recount the start of what is now four decades of the hollowing out of national, state, and local infrastructure to protect public health.
The inadequate preparedness and disorganized response to the pandemic are but two consequences of a long ideological struggle. On one side are believers that government has a primary Constitutional role to promote the general welfare. Think of the safety nets of FDR’s Social Security (and its subsidies for state unemployment insurance), LBJ’s Medicare, Medicaid, and Head Start, and BHO’s Affordable Care Act. On the opposing side are those who place faith in markets and voluntary charity to fulfill societal needs, advocating laissez-faire government shrunk to a size small enough figuratively to drown it in a bathtub.
Since President Reagan threw down the gauntlet in his 1981 inaugural, “… government is not the solution to our problem; government is the problem”, public health has suffered Sisyphean setbacks by on-again, off-again spending cuts, hiring freezes, and layoffs as each president proposes and Congress disposes. State and city health departments suffered as well, as Federal subsidies via CDC shrank and recessions reduced revenues and staff, often not fully restored when good times returned. On April 10th, the CDC director, Dr. Robert Redfield, acknowledged as much: “The reality is, for decades we’ve underinvested in public health,” he said. “So this is a time for us to reinvest heavily — get overpowered.”
Early Skirmishes
Ten years into the budget wars, one of us recalls admonishments by bean counters in Atlanta protecting tight budgets to stop approving timesheets with overtime for a lab chief dedicated to studies in Thailand of the explosive spread of the last deadly pandemic — HIV/AIDS — which was infiltrating the rest of Asia. Our solution was voluntary working off-the-clock (a Civil Service no-no) and pretending not to notice in late evenings a white lab coat, donned and in motion in front of a clicking keyboard.
A decade later another bleak era began, coinciding with early skirmishes of a parallel war on science. A Bush-II-appointed CDC director serving from 2002–2009 acceded to White House censorship of her testimony to Congress on the impact of climate change on health. She also led a disastrous major agency overhaul, accelerating lowered morale, sparking departures of senior experts, and prompting an unprecedented letter of concern from five former directors.
An untold skirmish in 2004 was CDC’s violation of its own Pledge to integrity, openness, and honesty. It staged a “Blue Ribbon Panel” of external members (including some anti-vaccine advocates) to consider calls by prominent academics (following internal grumblings) to remedy inherent conflicts of interest because its research on the adverse effects of vaccines occurs within programs promoting immunization (one of the greatest achievements of science and health).
Senior CDC leadership threatened that “heads would roll” if its vaccine-safety researchers communicated with the panelists. They withheld from the panel written evidence of undue interference prepared for it by the safety unit, most of whose researchers were barred from observing panel sessions.
Recent Battles
In recent years the budget wars heated up again, as reflected in proposed Trump administration cuts to CDC in the last four Presidential budgets. The most recent would start in October 2020 with a 15 percent reduction of $1.2 billion by slashing categories such as pandemic preparedness and response, occupational health (which certifies N95 masks), zoonotic diseases (of which COVID-19 is one), and global health (which puts CDC personnel in long-term assignments overseas to strengthen epidemic detection, control, and research by other countries).
One illustration of the strategic wisdom of such overseas activities was in 2014, when CDC staff assigned long-term in Nigeria helped it snuff out an outbreak of Ebola which had spread from its hot zone in West Africa (where over 1,400 other CDC staff served short tours of duty), averting catastrophic spread to the rest of Africa and probably beyond.
Casualties for COVID-19 Preparedness
Casualties affecting the current pandemic include recent drastic reductions of CDC’s U.S. epidemiologists and laboratorians posted in China before the appearance there of COVID-19 (Disclosure: CDC thus assigned one of us to China for 5 years until retirement in 2014). Those missing eyes, ears, and collegial relationships working alongside local scientists might have been able to notify Atlanta headquarters of what was happening in Wuhan a couple of weeks earlier than this past December 31.
Another casualty was removing CDC from primary management of the Strategic National Stockpile in 2018 to create “efficiencies”. How this shift may have affected SNS priorities and procurement requires after-action review. Trump recently claims he inherited a “broken” SNS with “empty shelves” and “bare cupboards”, but never explains why in the more than three years since, he did not fix it.
Problems with the CDC Test
Investigative reporting by Axios and the Washington Post revealed possible causes for initial problems with CDC’s original genetic test (pp. 6–55 of 80) for the SARS-CoV-2 pandemic virus, including lapses in proper segregation of lab spaces and processes that may have contributed to cross-contamination. But the scientists who developed the test are defenseless in remaining barred from writing or press interviews about these and other potential contributing factors.
Did senior management at CDC or in Washington rush them to get their test out the door in fewer than three weeks after the virus genome was announced in mid-January? Did the test’s PhD developers try to resist a premature release while not yet satisfied all necessary quality controls and validations were completed?
Were their development efforts hampered by years of PhD attrition and turnover, and current limitations in staffing, overtime, space for segregating processes, equipment, contracts, or other needed resources to complete their effort? In contrast to Trumanesque responsibility, will we see blame for the initial test deflected to CDC’s Respiratory Viruses Branch and other boxes sited quite low in the Federal organizational chart?
“Did protectionist pressures or scientific pride favor ‘our own’ tests … ?”
On April 9th, National Public Radio questioned the CDC director about problems with the test; his answers were non-responsive. Asked why the administration did not pursue simultaneously the “German test” (pp. 60–72 of 80), distributed early and widely by the World Health Organization, he deflected to the Food and Drug Administration. FDA has yet to provide answers. Did protectionist pressures or scientific pride favor “our own” tests, as the U.S. and France once fought in the 1980s over rival claims of ownership and royalties for HIV testing?
Challenges for Genetic Tests
Developing genetic tests by polymerase chain reaction (PCR) is challenging and takes time to get right. To minimize false-positive results, vials, equipment, and entire laboratories must all be kept scrupulously clean to avoid cross-contamination, which also applies to where specimens are collected from patients.
One of us, in developing the world’s first genetic test for HIV barred janitors from his CDC lab, so that he himself could carefully mop the floors and wipe surfaces to avoid stray virus genes wafting into the testing process. That test took many months for quality control and validation. Once ready, it finally permitted early diagnosis of infants born to HIV-positive mothers, and provided evidence that a Florida dentist with AIDS transmitted HIV to his patients.
CDC has long experience inventing diagnostic tests for numerous infectious diseases. Some are performed in-house as a reference service for its partners in state and local public health labs. Or it furnishes reagents and instructions to the partners themselves to test using their existing “low-throughput” machines.
Responsibility for Recruiting Industry
But the agency is not staffed nor equipped to customize processes, oversee reagent mass production, nor validate the proprietary, highly-automated systems made by outfits like Roche, Abbott, and Cepheid that are essential for the huge numbers of tests needed for a pandemic. Such machines are found in large, centralized clinical laboratories that, if sufficiently staffed around the clock, could perform a few thousand of such tests daily.
CDC awareness of the threat of spread from China prompted it to activate its emergency operations center on January 20th. That is when a national-level incident-command system should have been activated in Washington. One early task of such an ICS would have been to reach out in January, not March, to industrial collaborators to prepare for the predicted massive need of tests. In 2014, a prompt, government-wide effort coordinated the Ebola response that successfully kept that epidemic in Africa.
Accuracy in Testing
One critical issue about testing barely mentioned at White House briefings is that none of the many genetic tests to diagnose active infection in the U.S., or even others listed early by WHO, have yet to have any published studies of their accuracy in actual field use.
Such studies measure how well specimens collected in the real world and tested in typical clinical labs correctly identify true infection, termed “sensitivity” (100% means all truly infected are detected — i.e., no false-negative results). The converse measure is of true non-infection, “specificity” (100% means all truly uninfected are deemed so — i.e., no false positives). (For technical explanation, search these quoted terms and “PPV” and “NPV”.)
Confusingly, real-world sensitivity has an entirely different meaning than the “[analytical] sensitivity” reported by test developers for how often their assay can detect their claimed fewest number of viruses (e.g., 3 to 5) in contrived dilutions.
False positives and false negatives occur in nearly all medical testing. False positives may result from contamination by extraneous viral genes at various steps in specimen collection, transport, manual lab handling and processing, and within the machine. False negatives may result when swabs miss the optimal spot, are collected too early in the infection, or undergo lapses in transport or lab.
“… Senator Rand Paul’s coronavirus test … may have been a false positive …”
False-negative results are worrisome as the infected may not be isolated and thus unknowingly spread virus to others. Temporary isolation of false positives may be a personal inconvenience that society must tolerate. For example, Senator Rand Paul’s coronavirus test collected on March 16 may have been a false positive, given his age of 57 and never reporting any symptoms before or after announcing on April 7 a negative follow-up test. Only an accurate antibody test for COVID-19 can verify if Paul ever was truly infected.
Head-to-head comparisons by researchers independent of test manufacturers are needed to assess the performance of genetic tests. Such studies might use specimens collected in real-world conditions at clinics, hospitals, and drive-in sites, then assembled by investigators into blinded sets to include both the truly-infected and non-infected as determined by the best-available methods (e.g., virus culture, electron microscopy, subsequent antibody test). Such sets would then be sent to a sample of large and small clinical labs for external quality-assurance testing.
Tests found to perform poorly should have their emergency-use authorizations (EUAs) revoked by FDA. Publication of results would widen awareness of the fallibilities of all testing, including for antibody tests of which many now sold in the U.S. are of suspect accuracy, and for future antigen tests. Such data will promote procurement of more accurate products once sufficient supply allows such choice.
Dirty Epidemic Curves
Epidemiologists usually pay far more attention to the trends indicated by epidemic curves — changes in the timing and slopes of their rise, flattening, and fall — rather than the case numbers that generated them. Disease detectives speak of “dirty data”, not pejoratively, but only to indicate awareness of so many factors why counts of infections, deaths, and other metrics are but shadows of varying blurriness on the wall of Plato’s cave in reflecting what is really happening.
Data on the COVID-19 pandemic is especially dirty: Counts are pushed up or held down by many artifactual factors, which may change in degree over time. Confirmed cases move up as tests become more available and stall when needed swabs, reagents, kits, and staff to collect specimens diminish in supply. Counts spike up when out-of-hospital deaths are added to totals for those in whom post-mortem tests were skipped to preserve supply for the living.
Counts of confirmed infections fail to reflect the huge submerged part of the iceberg of those without symptoms or never tested. Death certificates may fail to mention unconfirmed COVID-19 triggers which fatally exacerbated underlying heart, lung, or diabetic disease. Some governors may be tempted to fudge or conceal the numbers of cases, deaths, and tests reported by their state. Some data are less dirty than others, such as overall hospital admissions (at least while elective procedures are cancelled and traffic trauma is minimal), and intubations of those about to be put on ventilators.
The nature of public health is that tough decisions must often be made with dirty data, and occasionally none at all. In emergencies, public health officials meld understanding of outbreak dynamics with experience in previous epidemics, plus a good bit of common-sense and “gut” intuition when novel pathogens arise. Tough tradeoffs are inevitable: School closings reduce childcare, keeping at home many essential workers.
Models Ignore Human Nature
Academic models which predict future curves of the epidemic may be useful in the short term as they update with fresh data. But many projected downslopes of the “tail” after the peak (Governor Cuomo’s “apex”) are misleadingly optimistic in decreasing steadily to zero within a few months. Why? Because the most important variables of all are not factored in: human nature and its fickleness. The remarkable public cooperation for many weeks that is flattening and pushing down curves in some areas may not be sustainable month after month after month.
As even a broken clock will indicate the truthful time twice a day, one must suspend routine disbelief in Trump’s statements to agree he is right: The country cannot remain locked-down interminably. Cracks are appearing in the supply of essential goods. Cabin fever, stir craziness, and economic hardship may contribute to declining compliance with stay-at-home orders and closures. But any such relaxation, either carefully managed or pell-mell by rebellious citizens, must be accompanied by frank public acknowledgements that illness and death will increase above any flat or declining levels achieved so remarkably by comprehensive lockdowns.
“The optimal titration is to achieve a roughly stable epidemic curve, which nowhere will be near zero.”
Metaphors for Mitigation and Relaxation
To understand how mitigation efforts might be relaxed, and with due respect to the explainer-in-chief, Dr. Fauci, it is more intuitive to flip his automotive metaphor. The closures and lockdowns have been like pushing a brake pedal almost to the floor, bringing to crawls both the human interactions that spread the virus and the economic life of the nation.
Another metaphor illustrates a prudent approach: Titration describes a chemist’s careful adjustment of conditions in the retort — amount of raw ingredients, enzyme concentration, flow of oxygen, degree of heating — all to keep a reaction at the desired rate. For COVID-19 the primary aim will be to titrate relaxations to keep hospitalizations below the graph’s red line representing overwhelmed hospital emergency rooms and intensive-care units, while resuming some economic activities with safe practices strictly enforced.
Titrating the epidemic will be far more difficult than for a simple chemical reaction. Dozens of factors will interact in complex ways affecting the resulting rate of transmission. The effects will be difficult to predict by academic modeling.
Thus, an empirical approach is required, with the patience to wait after each modest lift up on the brake to observe the effect. It may take 3 to 4 weeks for any resulting new infections to become apparent when some end up in hospitals or on mechanical ventilation. The optimal titration is to achieve a roughly stable epidemic curve, which nowhere will be near zero.
A paradoxical negative effect may influence the COVID-19 curves after the godsend when rigorous trials prove that a drug will interfere with the virus or blunt an overdriven immune response to substantially enhance recovery from illness. Regardless of probable long delays before drugs can be widely available, and their certain inability to save all patients, some may think, “So if I get it, no problem; I’ll take the medicine and be cured”. Then go out to celebrate, hugging and kissing in streets and bars.
To date, there is no evidence of any overall tapering down of the epidemic, which will likely continue well into 2021. We can only expect a generally downward slope over many months as increasing proportions of the population become immune, either by surviving natural infection or artificially by vaccination. This is the herd immunity that makes it harder for the virus to jump to a susceptible next person before it kills its current victim, or the victim’s immune system kills it.
Vaccines? Not So Fast
The degree and duration of such natural or artificial immunity (presumed to result but not yet proven), can only be determined by following large cohorts of persons after either a prior positive genetic test, or when a vaccine was received, and determining if and when they may be [re-]infected. This will require at least a couple of years of enhanced surveillance, and is absolutely essential in formal phase-III field-efficacy trials of candidate vaccines.
Dr. Fauci’s 12-to-18-month prediction for an effective vaccine is optimistically unprecedented, and Trump’s ”Warp Speed” schedule is recklessly dangerous. Pivotal trials with an unusually short period of follow-up might not detect serious adverse sequelae. For example, a phenomenon known as antibody-dependent enhancement causes some vaccine recipients, who nevertheless become infected by exposure to a pathogen, paradoxically to have more severe illness than if they had not been vaccinated at all
ADE has been observed for coronavirus vaccines in monkeys, pigs, cats, and in cultured human cells. It was also observed in children after a trial of a respiratory syncytial virus vaccine and after a mass campaign of a licensed dengue virus vaccine given to 830,000 children in the Philippines, resulting in withdrawal of the vaccine.
Adverse consequences detected after introduction of new influenza vaccines have included Guillian-Barré syndrome, Bell’s palsy, and narcolepsy. EUAs, by definition, bypass thorough regulatory review of how new vaccines (and drugs) are made and work. One famous example of lax Federal oversight was the famous “Cutter Incident” in which faulty production caused paralytic polio in some early vaccine recipients. Little known is that the problem was not limited to just one manufacturer, as documented by CDC in its secret 1955 “Wyeth Problem” and 1957 “Wyeth Report”.
Experience suggests three to four years is a more realistic timeframe to have a COVID-19 vaccine proven safe enough to put into many millions of healthy people. Consider the deadly Ebola epidemic in 2014 to 2016, during which the world barely dodged a bullet. In October 2014, the first phase-I vaccine trials began in American volunteers, with a succession of further trials.
The pivotal trial in Guinea and Sierra Leone ended in January 2016, having used a novel study design with only 84 days of follow-up. The vaccine was put to use in 2018 under EUA to vaccinate over 300,000 persons to control a later epidemic in Central Africa. In 2019, the FDA finally licensed the Ebola vaccine, warning that its duration of protection was unknown.
Even if the first COVID-19 efficacy trials were to be a “home run” in protecting, say, 90% of recipients, it may take a year or more to produce the hundreds of millions of needed doses (one per person? two? more?). An exception for such delay would be to emulate the financial gamble of FDR’s March of Dimes foundation in the 1950s. It paid for advance manufacture of 27 million doses of polio vaccine to be on hand in case the efficacy trial still underway would prove the vaccine worked. It did, and vaccination started within days of the famous announcement.
Vaccines never reach more than 95% of U.S. children and adolescents recommended for them, nor more than 75% of adults. Nor are vaccines ever 100% protective. Annually, 140 million humans susceptible to the SARS-CoV-2 virus causing COVID-19 are born on the planet, including 3.8 million in the U.S. The most probable scenario is that transmission of this virus will persist for years, becoming an endemic disease, as have many other emerging pathogens in recent decades.
The Banality of Guidelines
The White House, in obvious desperation as the election looms, rushed out its guidelines for relaxing mitigation efforts and lockdowns. Titled as a political slogan (“Opening Up America Again”), complete with campaign-logo bars, the guidelines are banal, quantitatively and subjectively vague, ambiguous, and shirk any Federal responsibility.
The guidelines are de facto an algorithm that artfully provides no diagram of sequential standard boxes connected with Yes and No arrows. Such clarity would reveal that even under their most indulgent interpretation, no state is anywhere near satisfying its “gating criteria” to proceed even to a box labeled “Phase One”.
To verify its “downward trajectories” of documented cases or percentages positive, the guidelines provide no minimal testing numbers per population to perform, nor the geographic extent for testing in a state. To satisfy its criteria for “syndromic” surveillance, it avoids specifying how many “sentinel sites” are needed in each state, nor how widely located they should be.
In burdening the states to solve the obvious shortages in testing, PPE, and contact tracing, the guidelines’ section entitled “Core State Preparedness Responsibilities” is vague whether its specified “Abilities” are criteria — Yes or No — necessary to pass to its Phase One.
Astonishingly, in requiring hospitals to “Treat all patients without crisis care.”, the guidelines are silent in defining what that means. Is “crisis care” when hospital workers cannot follow longstanding regulation and standards of care that PPE must be disposed after each contact with a patient in infectious-disease isolation? Its criterion “without crisis care” is clearly unsatisfied while health workers must wear N95 masks and gowns all shift long, or re-use them “off-label” for multiple days after decontamination under EUAs.
The guidelines also neglect to justify why a requirement for “robust testing” of healthcare workers does not apply as well to police, fire and ambulance crews, bus drivers, and so many other essential workers at risk by interacting with the increased numbers in public that its phases would permit.
“ … how many would answer phones that display, say, ‘County Public Health’? ”
Mustering the Troops
Both states and the country as a whole are estimated to need hundreds of thousands of case finders and contact tracers. This is orders of magnitude greater than the already busy employees that states and localities now have. Such work is made even more labor-intensive because U.S. telephones have lost much utility. With so many spam calls now spoofing caller IDs and numbers, how many would answer phones that display, say, “County Public Health”? Some propose mustering students, volunteers, or the equivalent of a Public Health Corps to do the job, as Massachusetts has begun. Until such armies can begin work, existing National Guard soldiers might deploy to back up health departments.
Natural Experiment
As any thinking person would have anticipated, Opening Up America Again is now serving as political cover for some states to relax whatever mitigation efforts were in place. Thus, the nation is entering what epidemiologists call a natural experiment. This is unlike proper scientific trials in which interventions such as drugs or their dosages, and placebos as controls, are allocated randomly to subjects (guinea pigs or consenting humans), with investigators and patients alike “blinded” to who gets what, to avoid biased assessments of results until the study is over.
In the unblinded natural experiment, the states and regional consortia of them are determining the onset, pace, and degree of their relaxations. Then experts will compare the illness and death that follow, taking into account as well the extent they achieve in testing, case isolation, and contact quarantine. To allow apples-to-apples comparisons, many confounders will need adjusting, such as age distribution, population density, commuting methods, and employment types.
Our admittedly crude approximation to observe the effect of “opening up” is to stratify by political preferences: red, purple, and blue (Figure). Densely-populated areas, mostly “blue”, were seeded early by imported virus and hit hard. Urban transportation systems with crowded buses and trains likely facilitated transmission. Nevertheless, comprehensive lockdowns put them onto downslopes of their curves. But the epidemic continues to spread inexorably in rural areas, mostly “red” states, with more dispersed populations, different commuting means (car and pickup), and other features that may slow but not eliminate transmission.
“ … governors may … be Pied Pipers leading some constituents into the folkloric river to drown.”
We defer to others to devise better ways to stratify the many differing degrees of relaxation to compare their effect on the counts of newly-diagnosed infections and deaths (e.g., anonymized tracking of smartphone movements). In any case, the resulting state and national epidemic curves will be as volatile as the recent stock market. Governors who “open up” their states too soon or too broadly may turn out to be Pied Pipers leading some constituents into the folkloric river to drown.
Damaged Reputations
Disheartening about the pandemic response is the damage to reputations, both institutional and personal. CDC’s logo was sullied when someone put it on the White House webpage and download of the Opening Up guidelines. Such labeling was defamatory on a document so unlike the thousands of well-defined, clearly explained recommendations and guidelines the agency has published under that logo, often cited and respected worldwide.
Even CDC’s investigations of COVID-19 outbreaks in meatpacking plants appear tainted by political interference. These insults must be shameful for CDC’s many professionals now working long hours, many off-the-clock, in doing their best with limited resources to carry out so many tasks to monitor and control the U.S. epidemic.
Sad as well is to watch the talented Dr. Birx who, like Anonymous, patriotically tries to mitigate damage to the nation by an unconstrained, certifiable, narcissistic sociopath. Like so many others drawn close to the Trump flame, her reputation has been singed. It is not the Debbie we know who answers questions with long-winded circumlocutions (at 56 and 67 minutes into the transcript of April 21st) about Georgia’s opening up of beauty, massage, and tattoo parlors, barber shops, etc. Why not simply reply?: “Such venues are incompatible with the new Opening Up guidelines. Period.”
“One cannot have a ‘second wave’ without a trough after the current first one, which shows no sign of ebbing (Figure).”
The next day, in responding about both influenza and COVID-19 “circulating at one time“ in the autumn, both she and the President prefaced answers with the hypothetical “if it comes [back]”. Such is happy-talk spin implying COVID-19 would be mostly gone before that season.
It required our living national treasure, Dr. Fauci, immediately to provide his unvarnished expectation, “There will be coronavirus in the fall.” [Period. emphasis added] One cannot have a “second wave” without a trough after the current first one, which shows no sign of ebbing (Figure).
The political rallies masquerading as coronavirus task force announcements in the White House briefing room now appear over. Going forward, both the good doctors ought demonstrate their integrity by refusing to be campaign props in standing beside and lending prestige to politicians running for re-election. If barred from their own separate White House press briefings with unfettered Q&As, so be it.
States can continue to manage the epidemics with their own teams of experts. Talented explainers can be brought back to the podium on January 20, 2021. After that date, CDC and so many other public institutions can begin to repair the damage, and the citizenry to seize the advantage in the war defending government.
— 30 —